19 Hidden Triggers of Leaky Gut That Could Be Fueling Your Hashimoto’s
Hey there, Hashimoto’s warrior! If you’re battling fatigue, brain fog, weight gain, or mood swings, you know how tough it can be to feel like yourself. As a licensed functional medicine nutritionist and certified nutrition specialist, I’ve helped countless women at Out of the Woods Nutrition break free from the grip of autoimmune thyroiditis to live vibrant, joyful lives. You’ve probably heard me talk about leaky gut—the sneaky condition where your gut’s lining lets toxins and food particles into your bloodstream, sparking inflammation that worsens Hashimoto’s. But what causes leaky gut? Today, we’re diving into 19 research-backed triggers that could be filling your “health bathtub” and keeping your symptoms stuck. My goal? Help you identify what’s driving your leaky gut so you can take action and reclaim your energy. Let’s do this!
The Bathtub Theory: Why Leaky Gut Happens
Think of your gut health as a bathtub. When it’s working well, your gut’s tight junctions—those tiny gates between cells—keep toxins and undigested food out of your bloodstream. But certain triggers act like water, filling up your bathtub until it overflows, causing leaky gut. For women with Hashimoto’s, this overflow fuels inflammation, confuses your immune system, and ramps up thyroid attacks. Rarely is there one “smoking gun”—it’s usually a combo of triggers piling up over time. The good news? You can drain that bathtub by addressing these triggers. I’ve grouped them into three buckets—medical history, food, and lifestyle—so you can pinpoint what’s affecting you. Grab a pen and jot down any that resonate as we go!
Bucket 1: Medical History Triggers
These are things from your past that you can’t change now but may still be impacting your gut. They’re like old leaks in your bathtub, quietly adding water.
1. Chronic Medication Use
Medications like nonsteroidal anti-inflammatory drugs (NSAIDs, e.g., ibuprofen), antibiotics, steroids, or acid-suppressing drugs (PPIs for reflux) can damage your gut lining. Studies show NSAIDs can cause leaky gut in just days, while antibiotics disrupt your microbiome, and PPIs impair digestion, feeding bad bacteria. If you’ve relied on these long-term, they’re likely a trigger.
2. Mercury Fillings or Heavy Metals
Mercury from dental fillings or heavy metal exposure (e.g., from industrial work) can inflame your gut, increasing permeability. If you have amalgam fillings or a history of chemical exposure, this could be a factor.
3. Traumatic Injuries
Traumatic brain injuries (TBIs) or severe physical trauma (like car accidents or burns) disrupt gut function. Research shows TBIs increase intestinal permeability, possibly via nervous system dysregulation. If you’ve had a significant injury, note it.
4. Chemotherapy or Radiation
Cancer treatments like chemo or radiation are tough on the gut, often causing leaky gut. If you’ve undergone these, they could still be affecting your gut health.
5. Cesarean Birth
Babies born via C-section miss out on the microbial exposure of vaginal birth, leading to altered gut bacteria and higher leaky gut risk. If you were a C-section baby, this might be a factor.
6. Gut Dysbiosis
Dysbiosis—imbalanced gut bacteria—is a huge trigger. This includes:
Bacterial Infections: Like Campylobacter, which can persist and cause leaky gut for over a year.
Parasites: Common in chronic gut issues or after food poisoning.
Small Intestinal Bacterial Overgrowth (SIBO): Bacteria in the wrong place (small intestine) release zonulin, a protein that opens tight junctions, just like gluten does.
Viral Infections: Like Epstein-Barr or Lyme disease, which keep inflammation high.
Lipopolysaccharides (LPS): Toxic byproducts from bacteria that widen tight junctions, letting toxins into your blood.
7. Hormone Imbalances
Hormones like thyroid, estrogen, progesterone, or testosterone regulate gut health. Low thyroid hormones (common in Hashimoto’s) or imbalanced sex hormones (e.g., from PMS or menopause) increase permeability. If you’ve got hormone issues, this is a big trigger.
8. Chronic Inflammation
Inflammation and leaky gut are a vicious cycle—each fuels the other. Conditions like gastritis or colitis signal gut inflammation, which widens tight junctions. If you’ve got any “-itis” condition, this is likely a factor.
Bucket 2: Food Triggers
What you eat can either heal or harm your gut. These triggers are like pouring water into your bathtub daily, but you have more control over them.
9. Nutrient Deficiencies
Low levels of vitamin A, zinc, magnesium, vitamin D, or calcium weaken tight junctions and slow gut repair. For example, vitamin D supports mucosal healing, and deficiencies (common in winter) increase leaky gut risk. If you’ve tested low or skimp on nutrient-dense foods, this is a trigger.
10. Gluten and Grains
Gluten, especially gliadin in wheat, is a top leaky gut trigger, even in non-celiac folks. It prompts zonulin release, opening tight junctions and causing inflammation. Other grains (like corn or rice) have similar proteins, called prolamins, that can be tough to digest. For Hashimoto’s, gluten also mimics thyroid tissue, worsening autoimmune attacks.
11. Genetically Modified Organisms (GMOs)
Emerging research shows GMO foods (common in processed products) damage the gut lining and disrupt microbiota in animal studies. If you eat a standard diet with non-organic corn or soy, GMOs could be a trigger.
12. Excess Sugar
Table sugar and processed sweets feed bad bacteria, especially in SIBO, boosting zonulin and leaky gut. Natural sugars in fruit are less concerning, but desserts and snacks are a problem.
13. Imbalanced Omega-6 to Omega-3 Ratio
A diet high in omega-6 fats (from seed oils like canola) and low in omega-3s (from fish or cod liver oil) fuels inflammation, worsening leaky gut. The standard American diet is often skewed this way.
14. Industrial Seed Oils
Oils like canola, soybean, or corn oil are high in omega-6s and processed with chemicals, making them inflammatory. They’re common in processed foods and restaurant cooking, adding to your leaky gut risk.
Bucket 3: Lifestyle Triggers
These daily habits can keep your gut inflamed, but they’re also areas where you can make big changes.
15. Sleep Deprivation
Getting less than 7-8 hours of sleep disrupts your circadian rhythm, suppresses digestion, and increases permeability. Studies show just 15-30 days of poor sleep can cause leaky gut.
16. Chronic Alcohol Use
Regular or binge drinking promotes SIBO and toxic byproducts like acetaldehyde and LPS, which open tight junctions. If you drink often, this is a trigger.
17. Chronic Stress
Physical stress (over-exercising, like marathon running), emotional stress (toxic relationships or trauma), or perceived stress (daily overwhelm) raises cortisol, weakening your gut. Studies show stress from public speaking or combat training increases permeability.
18. Overtraining
Intense exercise like CrossFit or marathons, done too often, acts like physical stress, boosting inflammation and leaky gut. If you’re pushing your body too hard, this could be a factor.
19. Liver Toxicity and Low Glutathione
Your liver’s antioxidant, glutathione, protects your gut lining. Low levels—caused by constipation, heavy metals, or alcohol—increase permeability. If you’re constipated or have toxin exposure, this is a trigger.
Your Next Steps to Heal
That’s a lot, I know! But don’t panic—you don’t need to tackle all 19 triggers at once. Healing leaky gut is a marathon, not a sprint. Count how many triggers apply to you (I had 15 when I was at my sickest!). Most women have a combo, like gluten, stress, and dysbiosis, piling up over time. Here’s how to start draining your bathtub:
Go Gluten-Free: Eliminate gluten 100% to reduce zonulin and thyroid attacks. Check labels for hidden sources.
Eat Nutrient-Dense Foods: Add liver (1-2 oz/week), bone broth, and organic veggies to support gut repair. Aim for 80-90% nutrient-dense meals.
Balance Your Microbiome: Include prebiotics (garlic, onions) and probiotics (yogurt, sauerkraut) to restore gut bacteria.
Prioritize Sleep: Aim for 7-8 hours nightly to stabilize your circadian rhythm.
Manage Stress: Try 10 minutes of deep breathing or yoga daily to lower cortisol.
Limit Medications: Use NSAIDs or antibiotics only when necessary. Ask about gluten-free alternatives.
Test for Hidden Triggers: Work with a practitioner to test for SIBO, infections, hormones, or toxins via stool, blood, or urine tests.
Support Detox: Boost glutathione with NAC or foods like broccoli. Address constipation with fiber and hydration.
Avoiding Overwhelm
It’s easy to fall into the “Google death spiral,” researching every trigger until you’re overwhelmed. Take a deep breath—you don’t need to fix everything today. Start with what you can control (diet, sleep, stress) and work with a practitioner to tackle deeper issues like infections or toxins. My approach, detailed in A Mind of Your Own, combines testing and personalized plans to get you thriving.
Call to Action: Ready to identify your leaky gut triggers and transform your Hashimoto’s journey? Book a consultation at www.outofthewoodsnutrition.com to create a tailored plan that drains your bathtub and boosts your energy. Listen to our latest Help for Hashimoto’s podcast for more gut-healing tips, and share your trigger list in the comments below.
You’ve got this, and I’m here to guide you to vibrant health!
Is a Leaky Gut Sabotaging Your Thyroid? Unlock Better Health with These Insights
As a woman with Hashimoto’s thyroiditis, you’re likely familiar with the frustration of fatigue, brain fog, weight struggles, and mood swings. But what if the root of these symptoms lies not just in your thyroid but in your gut? As a licensed functional medicine nutritionist and certified nutrition specialist, I’ve seen countless women transform their lives by addressing gut health. A groundbreaking 2020 study by Dr. Alessio Fasano reveals that “all disease begins in the gut,” particularly through a process called leaky gut, driven by a protein called zonulin. For those with Hashimoto’s, understanding this connection could be the key to reclaiming your energy and vitality. Let’s explore how a leaky gut impacts your thyroid and what you can do to heal.
The Leaky Gut-Hashimoto’s Connection
Hippocrates said 2,500 years ago, “All disease begins in the gut,” and modern science is catching up. Fasano’s research highlights that chronic inflammatory diseases (CIDs), like Hashimoto’s, stem from a triad: increased gut permeability (leaky gut), immune system overactivity, and gut microbiome imbalances, combined with genetic predisposition and environmental triggers. In Hashimoto’s, your immune system attacks your thyroid, but what sparks this? Leaky gut, where the intestinal barrier becomes permeable, allows dietary and microbial antigens to enter the bloodstream, triggering inflammation and autoimmunity.
The star player here is zonulin, a protein that controls tight junctions (TJs) in your gut’s lining. Normally, TJs act like gatekeepers, regulating what passes from your gut into your body. When zonulin levels rise—often triggered by gluten or bacterial overgrowth—these gates open too wide, letting in proteins, toxins, and bacteria that inflame your immune system. For Hashimoto’s patients, gluten is a major culprit, as it mimics thyroid tissue, leading to mistaken immune attacks. This process, called molecular mimicry, can worsen thyroid symptoms and perpetuate fatigue, hair loss, and joint pain.
Why Are We Seeing More Leaky Gut?
Fasano’s hygiene hypothesis explains why CIDs like Hashimoto’s are surging in industrialized countries. Our “too clean” lifestyles—think antibiotics, processed foods, and less microbial exposure—disrupt our gut microbiome, the community of bacteria that shapes immunity. This dysbiosis increases zonulin, weakening the gut barrier. Add environmental toxins like fluoride (in water) or endocrine disruptors (in plastics), and you’ve got a recipe for inflammation, especially if you’re genetically predisposed to autoimmunity.
In Hashimoto’s, this is critical. Your gut microbiome influences how your immune system tolerates or attacks “self” tissues like the thyroid. A leaky gut lets in antigens that confuse your immune system, amplifying thyroid damage. Studies show that zonulin levels are higher in autoimmune conditions like celiac disease (CD), type 1 diabetes (T1D), and even Hashimoto’s, often before symptoms appear.
Zonulin and Chronic Diseases
Zonulin’s role extends beyond Hashimoto’s to other CIDs:
Autoimmune Diseases: In celiac disease, gluten triggers zonulin, increasing gut permeability and inflammation. In T1D, high zonulin precedes beta-cell destruction. Inflammatory bowel disease (IBD) and multiple sclerosis (MS) also show elevated zonulin, with leaky gut driving systemic inflammation.
Metabolic Disorders: Obesity, type 2 diabetes, and non-alcoholic fatty liver disease correlate with high zonulin, as dysbiosis fuels inflammation via bacterial toxins like lipopolysaccharides (LPS).
Neurological Conditions: Autism, schizophrenia, and depression involve zonulin-driven leaky gut, leading to neuroinflammation. In MS, zonulin may also weaken the blood-brain barrier.
Cancers: Gliomas and hepatocellular carcinoma are linked to high zonulin, suggesting barrier dysfunction plays a role in tumor growth.
Aging: Higher zonulin in older adults correlates with inflammation and frailty, while lower levels in healthy centenarians suggest a link to longevity.
For Hashimoto’s, this means a leaky gut doesn’t just affect your thyroid—it can amplify systemic inflammation, worsening fatigue, mood, and even joint pain.
Healing Your Gut, Healing Your Thyroid
The good news? You can address leaky gut to support your thyroid health. Fasano’s research shows that targeting zonulin and gut health can reduce inflammation. A zonulin inhibitor, larazotide acetate, is in phase III trials for celiac disease and shows promise for other CIDs like Hashimoto’s by tightening gut junctions. While it’s not yet available, you can take action now with diet and lifestyle changes.
1. Eliminate Gluten
Gluten is a top zonulin trigger, especially for Hashimoto’s patients, as it mimics thyroid tissue. Go 100% gluten-free, checking labels for hidden sources like sauces or processed foods. A 2013 study found that a gluten-free diet reduced thyroid antibodies in Hashimoto’s patients.
2. Support Your Microbiome
A balanced microbiome lowers zonulin and inflammation. Include:
Prebiotics: Foods like garlic, onions, and asparagus feed beneficial bacteria.
Probiotics: Fermented foods (yogurt, kefir, sauerkraut) or a high-quality probiotic supplement can restore gut diversity.
Butyrate-Producing Foods: Fiber-rich foods like sweet potatoes support bacteria like Faecalibacterium, which reduce zonulin.
3. Reduce Toxins
Environmental toxins like fluoride, pesticides, and plastics (phthalates) disrupt your gut and thyroid. Use a water filter, choose organic produce, and swap plastic containers for glass to lower exposure. This is something I go over with my clients. It’s a key step to improving your health.
4. Boost Nutrient-Dense Foods
Nutrients like zinc, vitamin D, and omega-3s (from fish or cod liver oil, 1–2 tsp/day) support gut repair and immune balance. Include:
Bone broth: Rich in collagen to heal the gut lining.
Leafy greens: Provide fiber and micronutrients.
Egg yolks: Supply choline and EFAs for gut and thyroid health.
5. Manage Stress
Chronic stress, common in Hashimoto’s, raises zonulin and inflammation. Try mindfulness, yoga, or deep breathing (10 minutes daily) to calm your nervous system and support gut healing.
6. Test and Monitor
Work with a functional medicine practitioner to test zonulin levels (via serum ELISA, though results may need interpretation due to assay limitations) and assess gut dysbiosis (e.g., stool tests for LPS or bacterial toxins). This helps tailor your plan.
Your Path to Vibrant Health
A leaky gut doesn’t have to derail your Hashimoto’s journey. By addressing zonulin triggers like gluten, nurturing your microbiome, and reducing toxins, you can strengthen your gut barrier, calm inflammation, and ease thyroid symptoms. My approach, detailed in A Mind of Your Own, combines comprehensive testing (thyroid, gut, nutrients) with personalized diet and lifestyle plans to tackle root causes.
Ready to start healing? Book a consultation at www.outofthewoodsnutrition.com to create a tailored plan that gets you back to thriving. Listen to our latest Help for Hashimoto’s podcast wherever you get your podcasts for more gut-healing tips, and share your story in the comments below. Let’s rebuild your health, one gut-friendly step at a time!
Managing Glycemic Load: A Comprehensive Guide to Sweetener Choices and Health
In today’s food landscape, sweeteners are ubiquitous, shaping our diets and impacting our health in profound ways. From processed snacks to beverages, added sugars contribute significantly to glycemic load, affecting blood sugar regulation, gut health, and overall well-being. Understanding how to manage glycemic load and make informed sweetener choices is crucial for maintaining metabolic health, supporting digestive function, and reducing the risk of chronic conditions like type 2 diabetes. This blog post explores the types of sweeteners, their effects on the body, and practical strategies for reducing reliance on added sugars, with a focus on bio-individuality and long-term health.
Why Glycemic Load Matters
Glycemic load (GL) measures how a food affects blood sugar, factoring in both its glycemic index (GI) and the amount of carbohydrates in a serving (GL = GI × grams of carbohydrates ÷ 100). High glycemic load foods cause rapid blood sugar spikes, which can strain metabolic processes, promote insulin resistance, and exacerbate digestive issues, particularly in individuals with conditions like small intestinal bacterial overgrowth (SIBO) or candida overgrowth. Managing glycemic load is especially important for those with gluten-related disorders, as inflammation and gut dysbiosis often amplify metabolic challenges.
Reducing added sweeteners is a key strategy for lowering glycemic load. This not only stabilizes blood sugar but also supports the gut microbiome, reduces inflammation, and curbs cravings for hyper-palatable foods. Let’s dive into practical guidelines for managing sweetener intake and explore the science behind different sweetener types.
Guidelines for Reducing Sweetener Use
Reducing Added Sweeteners
The first step in managing glycemic load is minimizing reliance on added sweeteners. Here are actionable strategies:
Eliminate Unnecessary Sweeteners: Identify foods and beverages with added sugars (e.g., sodas, packaged snacks) and opt for unsweetened versions. For example, choose plain yogurt over flavored varieties and sweeten naturally with fresh fruit.
Uncover Hidden Sugars: Processed foods often contain hidden sugars under names like corn syrup, dextrose, or maltose. Reading ingredient labels helps identify these sources, allowing you to choose healthier alternatives, such as homemade versions with reduced sugar content.
Prioritize Whole Foods: Fresh fruits like berries or apples provide natural sweetness with fiber, vitamins, and minerals, reducing glycemic impact compared to refined sugars.
Use Natural Sweeteners Sparingly: Honey, maple syrup, and molasses offer trace nutrients and have been part of human diets for millennia. Use them in moderation to balance flavor and health benefits.
Recalibrating the Palate
Many people are accustomed to overly sweet foods due to the prevalence of hyper-palatable processed products. Gradually reducing sweetener use can reset taste preferences:
Incremental Reduction: Dilute sugary drinks with water or reduce sugar in recipes by 10–25% over time. For instance, cutting sugar in banana bread recipes often goes unnoticed while lowering glycemic load.
Patience Pays Off: Taste buds adapt within weeks, making less sweet foods more enjoyable and reducing cravings for intense sweetness.
Expanding Flavor Profiles
Diversifying taste experiences can reduce reliance on sweetness:
Explore Other Tastes: Incorporate sour (e.g., lemon juice), bitter (e.g., arugula), or umami (e.g., mushrooms, broth) flavors to enrich meals. Try sipping warm broth before dessert or eating a sour pickle during a sugar craving to shift taste perception.
Enhance Culinary Variety: Experimenting with herbs, spices, and savory ingredients creates satisfying dishes without relying on sugar.
Approaching Novel Sweeteners with Caution
Novel sweeteners, such as sugar alcohols or artificial substitutes, are often marketed as healthy alternatives, but their long-term effects are not fully understood:
Moderation is Key: Many alternative sweeteners lack extensive research on their impact on hormonal signaling, metabolism, and the gut microbiome.
Bio-Individuality Matters: Responses to sweeteners vary. Monitor symptoms like bloating, cravings, or metabolic changes to assess personal tolerance.
Types of Sweeteners and Their Impacts
Understanding the properties of different sweeteners helps in making informed choices. Below, we categorize sweeteners and explore their glycemic and health effects.
Caloric Sweeteners
Caloric sweeteners provide energy and include natural sugars like:
Sucrose (Table Sugar): A disaccharide of glucose and fructose (GI: 65), commonly found in processed foods.
Fructose: A monosaccharide in fruits, honey, and vegetables (GI: 25). While it has a low GI, its metabolism is complex (see below).
Other Natural Sugars: Honey, maple syrup, molasses, coconut sugar, agave nectar, corn syrup, and rice syrup contain varying ratios of glucose, fructose, and trace nutrients. Their glycemic impact depends on serving size.
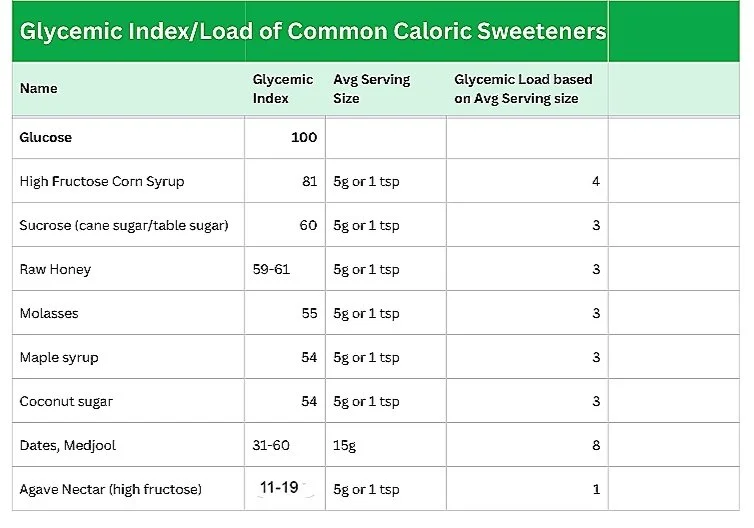
Glycemic Index/Load of Common Caloric Sweeteners
Serving size significantly affects glycemic load. For example, a 16 oz can of Coca-Cola contains 52g of high fructose corn syrup, far exceeding the 5g serving size used in GL calculations, leading to substantial blood sugar spikes despite its low GL rating.
Natural Non-Caloric Sweeteners
These plant-based sweeteners provide intense sweetness without calories:
Stevia: Derived from Stevia rebaudiana, stevia’s steviol glycosides are 200–400 times sweeter than sugar (GI/GL: 0). Whole leaf stevia offers antioxidant, antimicrobial, and anti-inflammatory properties (Papaefthimiou et al., 2023). Studies suggest stevia has minimal impact on insulin and may improve pancreatic beta cell function in type 2 diabetics.
Monk Fruit Extract (Luo Han Guo): Contains mogrosides, providing calorie-free sweetness (GI/GL: 0). Note that many stevia and monk fruit products include sugar alcohols like erythritol as the primary ingredient.
While these sweeteners don’t raise blood glucose, they may influence appetite-regulating hormones in some individuals, though evidence suggests minimal impact.
Sugar Alcohols (Polyols)
Sugar alcohols, such as xylitol, erythritol, and sorbitol, are carbohydrates with a lower glycemic impact due to partial absorption:
Xylitol: Slightly increases glucose and insulin but is effective in reducing cavities when used in gums or mouthwashes.
Erythritol: Highly absorbed and excreted in urine, causing fewer digestive issues (tolerance: ~0.66 g/kg/day for men, 0.80 g/kg/day for women; Mazi & Stanhope, 2023). It may induce satiety hormones like cholecystokinin.
Sorbitol: More likely to cause digestive upset due to poor absorption.
Glycemic Index/Load of Common Sugar Alcohols
Sugar alcohols act as prebiotics, potentially increasing beneficial bacteria like bifidobacteria, but excessive intake can cause bloating, diarrhea, or gas, especially in IBS/IBD patients. One study linked erythritol to increased gut inflammation in mice models of IBD (Jiang et al., 2023).
Inulin
Inulin, a prebiotic fructan, contains non-absorbable calories and has no glycemic impact. Found in chicory root, onions, bananas, and asparagus, it supports gut health by promoting beneficial bacteria and may improve glycemic control and lipid profiles in type 2 diabetics (Dehghan, 2012). It’s used in low-sugar products and probiotic supplements.
Artificial Non-Caloric Sweeteners
Synthetic sweeteners like aspartame, sucralose, saccharin, and acesulfame potassium provide intense sweetness without calories but pose health risks:
Health Concerns: Research links artificial sweeteners to impaired glycemic responses, glucose intolerance, and reduced gut barrier function (Shil et al., 2020). Aspartame is a potential carcinogen, and some studies suggest pathogenic microbiome changes (Ruiz-Ojeda et al., 2019).
Recommendation: Avoid artificial sweeteners due to their potential metabolic and gut health impacts.
Special Considerations
Hormonal and Satiety Effects
Sweeteners influence hormones like insulin, cholecystokinin, and glucagon-like peptide-1, which regulate blood sugar and satiety:
Erythritol and Xylitol: Promote satiety by slowing gastric emptying, aiding glycemic control.
Stevia: May improve insulin sensitivity without significant insulin spikes.
Low Insulin Response: While beneficial for reducing insulin resistance, low insulin can reduce leptin release, potentially increasing appetite and caloric intake.
Digestive Health
Sugar alcohols, particularly sorbitol and xylitol, can cause digestive upset due to fermentation in the gut. Erythritol is better tolerated, but IBS/IBD patients may be more sensitive. Inulin supports gut health, while artificial sweeteners may disrupt the microbiome.
GMOs and Consumer Preferences
Most erythritol is derived from GMO cornstarch, which may not align with preferences for non-GMO foods. Always check labels for transparency.
Understanding Fructose
Fructose, with a GI of 25, is often considered a low-GI sweetener, but its metabolism presents unique challenges:
Liver Metabolism: Unlike glucose, which is used by all cells, fructose is metabolized by the liver, where high doses can promote insulin resistance, triglyceride production, and uric acid buildup, linked to hypertension, kidney stones, and gout (Gugliucci, 2017; Sigala et al., 2021).
Appetite Regulation: Fructose stimulates less insulin and leptin than glucose, potentially increasing appetite and contributing to metabolic syndrome.
Fruit vs. Processed Fructose: Whole fruits have low fructose content (e.g., 8–10g in an apple) and fiber, minimizing glycemic impact. In contrast, a 16 oz glass of grape juice contains 37.2g of free fructose, causing rapid absorption and metabolic strain.
Insert chart here: Common Names for Refined Sugar in Ingredient Labels
Other names for refined sugar
Allulose, a rare sugar derived from fructose, shows promise for improving glucose tolerance but requires further research. It’s approved in the U.S. but not in the EU or Canada.
Practical Tips for Selecting Sweeteners
Read Labels Carefully: Products labeled “stevia” or “monk fruit” often contain sugar alcohols like erythritol. Check ingredient lists for accuracy.
Mix Sweeteners: Combine caloric (e.g., honey) and non-caloric (e.g., stevia) sweeteners to balance flavor, glycemic load, and satiety. For example, halve the honey in a recipe and add a pinch of stevia.
Monitor Bio-Individuality: Track symptoms like bloating, cravings, or metabolic changes after consuming sweeteners. Some individuals report that alternative sweeteners hinder weight loss or perpetuate cravings.
Contextualize Health Claims: A sweetener’s benefits depend on what it replaces. For type 2 diabetics, stevia may reduce cardiometabolic risks compared to fructose, but it’s not inherently health-promoting for all.
Integrating Sweetener Management with Digestive Health
Reducing glycemic load supports digestive health, particularly for those with gluten sensitivities, SIBO, or candida overgrowth, as high-sugar diets exacerbate dysbiosis. A low-sugar, whole-food-based diet, combined with prebiotics like inulin, can restore gut balance. For example, incorporating unsweetened yogurt with fruit and a sprinkle of inulin can nourish beneficial bacteria while keeping glycemic load low.
Practitioners can create resources like handouts listing hidden sugars and low-GI alternatives to guide clients. Personalized dietary reviews help identify high-sugar foods and suggest substitutions, enhancing compliance and outcomes.
Conclusion
Managing glycemic load through informed sweetener choices is a powerful tool for optimizing metabolic and digestive health. By reducing added sugars, prioritizing whole foods, and cautiously incorporating natural non-caloric sweeteners or sugar alcohols, individuals can stabilize blood sugar, support gut health, and reduce inflammation. Bio-individuality and context are key—monitor personal responses and consult practitioners for tailored guidance. With these strategies, you can enjoy sweetness in moderation while fostering long-term wellness.
How Essential Fatty Acids Impact Your Thyroid Health: A Game-Changer for Women with Hashimoto’s
As a woman navigating the challenges of Hashimoto’s thyroiditis, you’re no stranger to fatigue, brain fog, hair loss, or mood swings. You’re working hard to reclaim a vibrant, fulfilling life, but could a tiny nutrient group—essential fatty acids (EFAs)—be a missing piece in your healing journey? As a licensed functional medicine nutritionist and certified nutrition specialist, I’ve spent years helping women like you optimize their health through diet and lifestyle. This post challenges mainstream views on EFAs and offers insights that can transform how we support thyroid health. Let’s dive into why EFAs matter, how they affect Hashimoto’s, and practical steps to balance them for energy, clarity, and vitality.
What Are Essential Fatty Acids, Really?
You’ve likely heard that omega-3 and omega-6 fatty acids are “essential” for health. But the truth is more nuanced. Mainstream nutrition often labels linoleic acid (omega-6, found in vegetable oils) and alpha-linolenic acid (ALA, found in flaxseed) as essential because the body can’t make them. However, studies from the 1920s to today, shows that only two fatty acids are truly essential for preventing deficiency symptoms: arachidonic acid (omega-6) and docosahexaenoic acid (DHA, omega-3). These are critical for skin health, fertility, growth, and brain function—issues that hit close to home if you’re managing Hashimoto’s.
Here’s the catch: your body can make arachidonic acid and DHA from linoleic acid and ALA, respectively, but this process depends on your nutritional status, genetics, and stressors like inflammation or insulin resistance—common in Hashimoto’s. If these are off, you may need direct sources of arachidonic acid (from animal fats like liver) and DHA (from fish or cod liver oil). Otherwise, you risk symptoms like scaly skin, hair loss, or even worsened mood and cognition, which can feel like a thyroid flare-up.
Why Standard Advice Misses the Mark
Textbooks often claim you need 1–4% of calories from EFAs, but this is inflated by flawed studies using sugar-heavy diets or purified oils. Analysis of the research shows the real requirement is tiny—less than 0.5% of calories from animal fats like butter or lard, and just 0.12% from liver during growth or pregnancy. For women with Hashimoto’s, a nutrient-rich diet with liver, egg yolks, or butter from grass-fed animals can meet these needs effortlessly. Why liver? It’s packed with preformed arachidonic acid, DHA, and vitamin B6, which boosts EFA synthesis, reducing your body’s demand.
Surprisingly, eicosapentaenoic acid (EPA), the omega-3 in fish oil, isn’t a normal part of the mammalian body and may even disrupt arachidonic acid’s functions when overconsumed. High doses of fish oil (e.g., 4 g/day) can lower triglycerides, but this is a pharmacological effect, not a nutritional necessity, and may interfere with thyroid-supporting pathways. For Hashimoto’s, where inflammation and oxidative stress are already high, piling on EPA could backfire.
The Oxidative Stress Trap
Polyunsaturated fatty acids (PUFAs), including EFAs, are prone to oxidation due to their chemical structure. In Hashimoto’s, oxidative stress—driven by inflammation, nutrient deficiencies, or toxins like fluoride—can amplify damage from excess PUFAs. Masterjohn clarifies that PUFAs don’t cause oxidative stress but become a liability when stress is present, leading to damage in tissues like the liver or blood vessels. For example, short-term PUFA intake may reduce liver fat, but long-term excess can worsen nonalcoholic fatty liver (NASH), a concern for women with thyroid-related metabolic issues.
Heart disease data is equally eye-opening. While short-term trials show PUFAs like fish oil may lower cholesterol, longer trials (over 4 years) link them to a 30% increased risk of heart disease mortality. Vegetable oils, high in linoleic acid, also raise cancer risk in animal studies. For Hashimoto’s patients, who often face higher cardiovascular risks, minimizing PUFAs from vegetable oils and favoring animal fats is crucial.
The Thyroid-EFA Connection
Hashimoto’s often involves nutrient deficiencies (e.g., vitamin B6, biotin, zinc) that impair EFA synthesis, increasing your need for direct sources like liver or egg yolks. Chronic inflammation and stress, hallmarks of autoimmune thyroiditis, also heighten oxidative stress, making excess PUFAs a liability. For example, gluten, a known thyroid trigger, can mimic thyroid proteins, ramping up immune attacks and EFA demands. Birth control pills, fluoride, and endocrine disruptors (like phthalates) further stress the thyroid-adrenal axis, potentially depleting EFAs.
Findings suggest that a whole-foods diet low in sugar and rich in B6, biotin, and minerals can slash EFA needs, stabilizing thyroid function and mood. Cod liver oil (1–2 tsp/day) can support pregnancy or lactation, but overuse risks EPA overload, which may disrupt arachidonic acid’s role in skin and immune health—key for Hashimoto’s management.
Practical Steps for Hashimoto’s Warriors
Here’s how to optimize EFAs for your thyroid health:
Prioritize Animal Fats: Include liver (1–2 oz/week), egg yolks (2–4/day), and grass-fed butter or lard in your diet. These provide arachidonic acid and DHA without excess PUFAs.
Limit Vegetable Oils: Avoid PUFA-rich oils like corn, soy, or canola, which increase oxidative liability and compete with DHA synthesis.
Use Cod Liver Oil Sparingly: For pregnancy or lactation, 1–2 tsp/day provides DHA and vitamins A and D. For children, try ¾ tsp, per Weston Price’s protocol. Balance with arachidonic acid-rich foods like red meat, poultry, eggs and full fat dairy if you tolerate it.
Boost Nutrient Cofactors: Eat B6-rich foods (bananas, poultry) and biotin-rich foods (liver, eggs) to support EFA synthesis. Avoid sugar to lower EFA needs.
Monitor Symptoms: Scaly skin, hair loss, or infertility may signal EFA deficiency, especially if you’re vegetarian or low on animal fats. Consult a functional medicine practitioner to adjust your diet. I can help you with that.
Address Stress and Toxins: Minimize fluoride (use filtered water), avoid endocrine disruptors (check cosmetics), and manage stress to support adrenal-thyroid balance.
Your Path to Vibrant Health
EFAs are a small but mighty piece of the Hashimoto’s puzzle. By focusing on whole foods like liver and egg yolks, limiting PUFA-heavy oils, and supporting your body with key nutrients, you can reduce inflammation, stabilize mood, and boost energy. My approach combines comprehensive testing (thyroid, CBC, Comprehensive Metabolic Panel, Cholesterol, Iron panel, and more) with tailored diet and lifestyle changes to address the root causes of your symptoms.
Ready to take charge? Book a consultation at www.outofthewoodsnutrition.com to create a personalized plan that gets you off the couch and back to thriving. Check out our latest Help for Hashimoto’s podcast wherever you listen to podcasts for more tips, and share your journey in the comments below. Let’s unlock your vitality together! Be sure to sign up for my newsletter below and get the Definitive Guide to Hashimoto’s.
Nutrition for Every Stage of Adulthood: A Simple Guide.
As a functional medicine nutritionist supporting women with chronic illness and thyroid issues, I’m excited to explore how nutrition supports your health through different stages of adulthood. While everyone’s needs are unique (hello, bio-individuality!), your life stage—whether you’re in your 30s, 50s, or beyond—shapes your nutrient priorities. Let’s break down the key considerations for adulthood and older years, with practical tips to fuel your body for energy, resilience, and long-term wellness.
Nutrition in Adulthood (20s to 50s)
Adulthood is the longest life stage, packed with milestones like career growth, starting a family, or caring for aging parents (the “sandwich generation”). Your body’s growth stabilizes, so energy needs depend on factors like activity level, body size, gender, and health rather than rapid development. For women with thyroid issues or chronic conditions, nutrition plays a key role in managing symptoms and preventing future health challenges.
Key Nutrition Goals
Prevent Chronic Disease: Healthy eating now reduces risks of heart disease, diabetes, and osteoporosis later.
Manage Stress: Nutrient-dense foods support your body through busy, high-pressure years.
Maintain Energy: Balanced meals keep you fueled for work, family, and personal goals.
Macronutrient Needs
Your ideal balance of carbs, protein, and fats varies based on your lifestyle. For example:
Active adults (e.g., runners) may need more carbs (50-60% of calories) for energy.
Those with thyroid issues may benefit from higher protein (25-35%) and fats (30-40%) for stable energy. Use a food journal to track how meals affect your energy, mood, and fullness, then tweak portions. A typical adult needs about 2000-2500 calories/day, but this drops if you’re less active or have a slower metabolism.
Micronutrient Focus
Micronutrients are your body’s defense system, protecting against aging and disease:
Omega-3 Fatty Acids: Found in salmon, walnuts, or chia seeds, they lower heart disease risk and support brain health.
B Vitamins (B6, B12, Folate): Break down homocysteine (a heart disease risk factor). Eat eggs, leafy greens, or fortified grains.
Calcium: Strengthens bones to prevent osteoporosis. Get it from dairy, sardines, or kale.
Fiber: Keeps digestion smooth, stabilizes blood sugar, and supports weight management. Try oats, beans, or berries.
Antioxidants/Phytochemicals: Neutralize harmful free radicals. Load up on colorful fruits and veggies like blueberries or spinach.
Hydration
Your body is ~60% water, and you need 2-3 liters/day (about 8-12 cups) from drinks and foods. This varies with weight, activity, and climate. Sip water throughout the day, and eat water-rich foods like cucumbers or watermelon.
Practical Tips
Meal Idea: Grilled chicken with quinoa and roasted veggies (carbs, protein, fiber) drizzled with olive oil (healthy fats).
Snack: Greek yogurt with berries and chia seeds for protein, antioxidants, and omega-3s.
Lifestyle: Manage stress with mindfulness or walks to support nutrient absorption.
Track: Use myfooddata.com to check nutrient balance if you’re managing a condition like hypothyroidism.
Tip: Prioritize whole foods over processed snacks to build a strong foundation for health in your 40s and 50s.
Nutrition in Older Adulthood (65+)
As you enter your 60s and beyond, your body changes, and so do your nutrition needs. Life expectancy is rising, and older adults are a growing group with unique health challenges. Slower cell turnover, reduced digestion, and hormonal shifts can affect how your body uses nutrients, while chronic conditions or medications may increase specific needs. The goal? Maintain vitality, protect against disease, and support quality of life.
Key Nutrition Goals
Preserve Muscle and Bone Health: Counter age-related muscle loss (sarcopenia) and bone thinning.
Support Digestion: Maximize nutrient absorption despite reduced stomach acid.
Reduce Inflammation: Manage overactive immune responses that cause systemic inflammation.
Stay Hydrated: Prevent dehydration, which is riskier due to a weaker thirst signal.
Energy Needs
Calorie needs drop by ~5% per decade due to slower metabolism, less activity, and lower thyroid function. A 70-year-old may need 1500-2000 calories/day compared to 2000-2500 in their 50s. However, micronutrient needs stay high or increase, so focus on nutrient-dense foods (more nutrients, fewer calories).
Macronutrient Needs
Carbohydrates: Choose complex carbs (legumes, whole grains) for energy and fiber. Aim for 45-60% of calories.
Protein: Vital to preserve muscle. Aim for 20-30% of calories (1.0-1.2g/kg body weight) from lean sources like fish, eggs, or tofu. For a 70 kg person, that’s 70-84g/day.
Fats: Include healthy fats (20-30% of calories) like olive oil or nuts, but monitor saturated fats if heart health is a concern.
Micronutrient Focus
Older adults need extra attention to these nutrients:
Calcium, Vitamin D, Vitamin K: Protect bones against osteoporosis. Get calcium from dairy or fortified plant milk, vitamin D from sunlight or salmon, and vitamin K from spinach.
Antioxidants (Vitamins C, E, Carotenoids): Support vision and reduce oxidative stress. Eat citrus, nuts, or carrots.
B Vitamins (B12, Folate, B5): Boost brain health and cognition. B12 absorption drops with age, so include fortified foods or supplements (check with a doctor). Find folate in lentils or greens.
Omega-3 Fatty Acids: Ease joint pain and slow cognitive decline. Try fatty fish or flaxseeds.
Fiber: Promotes bowel health, often a concern. Aim for 21-30g/day from beans, oats, or apples.
Hydration
Dehydration is a serious risk as thirst sensation weakens. Aim for 2-3 liters/day of water, including from soups, broths, or fruits like oranges. Keep a water bottle handy and sip regularly.
Challenges and Solutions
Reduced Appetite: Smaller, frequent meals with nutrient-dense foods (e.g., smoothies with spinach, yogurt, and berries).
Digestive Issues: Soft, cooked foods (e.g., steamed veggies) or probiotics may help.
Sensory Loss: Enhance flavors with herbs to make meals appealing.
Medications: Some interfere with nutrient absorption (e.g., folate). Work with a nutritionist to adjust your diet.
Practical Tips
Meal Idea: Baked salmon, mashed sweet potato, and steamed broccoli for protein, carbs, and vitamins.
Snack: Apple slices with almond butter for fiber and healthy fats.
Hydration: Start the day with warm lemon water and eat soups or juicy fruits.
Track: Use a food journal to ensure enough protein and micronutrients, especially if appetite is low.
Tip: Add a handful of nuts to meals for extra protein and omega-3s to support joints and brain health.
A Holistic Approach
Nutrition is a lifelong journey, and every stage of adulthood calls for a nutrient-dense diet tailored to your unique needs. For women with chronic illness or thyroid concerns, focusing on whole foods, hydration, and micronutrients can boost energy, reduce inflammation, and set the stage for vibrant health. Stay tuned for more on digestion and personalized wellness strategies!
Ready to nourish your body at any age? Contact me for personalized functional medicine guidance.